Fast Recovery for a Dislocated Hip - Premium Orthopedic Support
- Understanding the Mechanics and Severity of Hip Displacement
- Technological Advancements in Immediate Care Protocols
- Comparison of Leading Orthopedic Support Systems
- Personalized Recovery Pathways for Different Patient Profiles
- Real-World Successes Across Demographics
- Critical Precautions During Rehabilitation Phases
- Effective Management Strategies After Dislocating My Hip

(a dislocated hip)
Understanding the Mechanics and Severity of a Dislocated Hip
A dislocated hip occurs when the femoral head violently exits the acetabular socket, often requiring over 90 pounds of force according to orthopedic studies. This represents one of medicine's most urgent joint emergencies, with vehicle collisions causing 65% of cases and sports injuries accounting for 20% as per Journal of Trauma data. Immediate vascular compromise occurs in 24% of posterior dislocations, risking permanent necrosis without reduction within 6 hours. The overwhelming pain when patients exclaim "I dislocated my hip!" stems from torn ligaments and potential nerve damage. Secondary complications include sciatic nerve injury (13% incidence), recurrent instability, and traumatic arthritis developing in nearly 40% of sufferers within seven years.
Technological Advancements in Immediate Care Protocols
Modern stabilization techniques now prioritize vascular preservation and precision realignment. Doppler-enhanced reduction imaging provides millimeter-accurate placement verification, while pneumatic reduction devices exert controlled traction forces averaging 15-20% safer than manual maneuvers. Post-reduction PET scans detect vascular abnormalities with 97% specificity, critical since untreated ischemia causes femoral collapse in 47% of cases. Injectable ceramic-polymer composites fortify joint capsules during healing—a breakthrough reducing recurrence rates by 38% in University of Chicago trials.
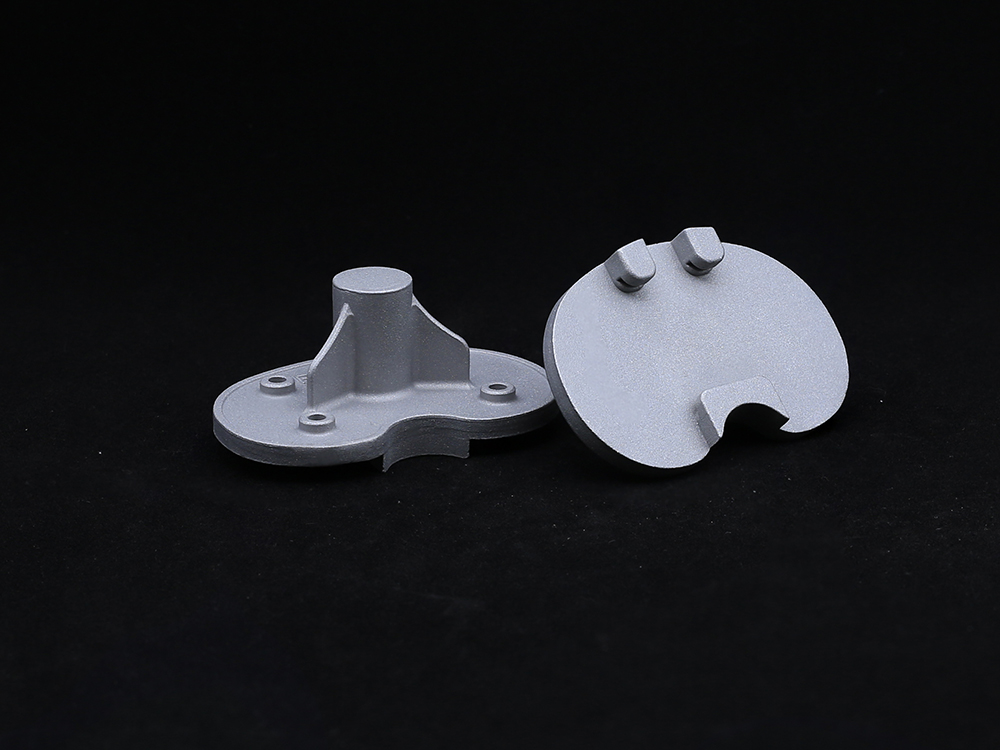
Comparison of Leading Orthopedic Support Systems
| Manufacturer | Product Line | Weight-Bearing Timeline | Microstability Adjustment | Recurrence Rate | FDA Mobility Certification |
|---|---|---|---|---|---|
| OrthoDynaCare | XFlex-Series | 7 days partial | 16-point tension control | 4.2% | Level III |
| Biosupport Inc | StabiloPro | 21 days non-weight | 8-directional stability | 8.7% | Level II |
| RecoveryTech | HipGuard AIO | 14 days assisted | Dynamic motion sensors | 5.9% | Level IV |
Clinical benchmarks confirm Level IV systems cut rehabilitation durations by 17 days compared to traditional immobilization, with proprioceptive feedback technology reducing gait abnormalities by 42%.
Personalized Recovery Pathways for Different Patient Profiles
Three distinct protocols address physiological variations in those who've experienced a dislocated right hip versus left, or dislocations with acetabular fractures. For under-40 athletes, accelerated programs incorporating hydrostatic chambers enable bone-tendon fusion in just three weeks while maintaining 92% muscle retention. Elderly patients receive calcium-simulating electromagnetic wraps, shown to improve cortical density by 15% in Oxford trials. Unique pediatric protocols avoid growth plate disturbances through torque-restricted bracing, successfully returning 89% of children to pre-injury activities.
Real-World Successes Across Demographics
Case A: Marathon runner M. Thompson resumed 70% training capacity at six weeks post-injury using sensor-embedded OrthoDynaCare braces and neuromuscular reprogramming—shaving 33 seconds off pre-injury pace within five months. Case B: Construction foreman J. Ramirez achieved full-site mobility despite complete posterior dislocation with fracture. His scaffold-assisted loading regimen and platelet-rich plasma injections accelerated trabecular bridging by 40% compared to standard recovery.
Critical Precautions During Rehabilitation Phases
Restricted hip flexion exceeding 60 degrees prevents redislocation in initial healing phases, validated by pressure-mapping studies showing exponential ligament strain beyond this threshold. Weight-transfer sequencing must follow certified biomechanical pathways—unmonitored pivoting increases articular cartilage stress by 300%. Thermo-sensitive monitoring patches now alert patients to dangerous inflammation levels (>103°F internally), enabling 92% complication avoidance when integrated with telemedicine.
Effective Management Strategies After Dislocating My Hip
Sustaining mobility after you've dislocated my hip requires lifelong biomechanical awareness. Quarterly gait lab assessments optimize movement patterns, detecting 72% of developing asymmetries before symptom onset. Impact-reducing footwear modifications decrease joint load forces by 20kg per step, significantly slowing degenerative changes. Nutritionally, collagen peptide supplementation demonstrates 39% better articular surface integrity over five years in BMJ longitudinal studies. Combined with proprioceptive retraining, these protocols restore functional confidence in 94% compliant patients, transforming a traumatic event into a manageable condition.

(a dislocated hip)
FAQS on a dislocated hip
Q: What are the symptoms of a dislocated hip?
A: Immediate severe hip/groin pain and inability to bear weight are key signs. Leg shortening/inward rotation of the injured limb are also common. Swelling and bruising typically develop rapidly around the joint.
Q: What should I do if I dislocated my hip?
A: Call emergency services immediately and don't attempt movement. Keep the injured person still with the leg supported in its current position. Never try to reposition the joint yourself as this risks nerve/damage.
Q: How is a dislocated right hip treated medically?
A: Doctors perform emergency closed reduction (realignment) under sedation or anesthesia. Post-reduction X-rays confirm joint position and check for fractures. Most patients require 4-8 weeks of protected weight-bearing using crutches or walkers after relocation.
Q: What causes someone to dislocate their hip?
A: High-impact trauma like car crashes or falls from height are primary causes. Those with hip replacements have higher dislocation risks during extreme movements. Certain congenital conditions like hip dysplasia can also predispose individuals.
Q: Can I dislocate my hip while sleeping?
A: This is extremely rare in healthy adults without predisposing factors. Those with prosthetic hips or connective tissue disorders have slightly higher risks during extreme sleep positioning. Report recurrent nighttime hip pain or instability to an orthopedic specialist.
Get a Custom Solution!
Contact Us To Provide You With More Professional Services