Precision Medial Femoral Condyle & Plateau Knee Implants
- Exploring condyle and plateau
anatomy and clinical significance - Quantifying the socioeconomic impact of knee injuries
- Comparing materials and technology in joint reconstruction
- Vendor capabilities for femoral condyle solutions
- Personalized treatment pathways and 3D-imaging innovations
- Clinical case review: Left medial femoral condyle restoration
- Advancements in knee preservation technologies

(condyle and plateau)
Understanding Condyle and Plateau Structures in Knee Pathology
The condyle and plateau form the primary articulation surface between femur and tibia, absorbing up to 5x body weight during ambulation. Medial femoral condyle fractures account for 55% of complex knee injuries according to AO Foundation data, with subchondral bone density varying significantly between lateral (mean 625 Hounsfield units) and medial regions (782 HU). Cadaveric studies demonstrate 3.2mm average cartilage thickness over the weight-bearing surfaces, explaining why osteochondral defects frequently occur here. Vascular penetration analysis reveals the medial condyle receives only 15-20 terminal vessels versus 30-40 in lateral regions, contributing to 68% non-union rates in central defects exceeding 2cm².
The Socioeconomic Burden of Condylar Injuries
Annual healthcare expenditures for condyle and plateau fractures exceed $4.7 billion in North America alone. Workers' compensation data indicates 42% of these injuries result in vocational disability, with laborers experiencing 7.3-month average recovery periods. Medicare claims analysis shows revision surgery rates climb to 31% when initial reduction leaves >2mm articular step-off. Longitudinal studies demonstrate accelerated osteoarthritis progression in 79% of patients with residual joint incongruity, resulting in average TKA advancement by 8.4 years. Post-traumatic arthroplasty cases cost 127% more than primary replacements according to AAOS economic reports.
Material Science Breakthroughs in Joint Reconstruction
Third-generation biphasic scaffolds now achieve 92% pore interconnectivity versus 78% in earlier designs, accelerating osseointegration. Nano-hydroxyapatite coatings demonstrate 3.8x greater osteoblast adhesion versus traditional titanium surfaces. Topography-mimicking implants manufactured through electron beam melting reproduce trabecular patterns within 12μm accuracy. Polyetherketoneketone (PEKK) composites now match cortical bone's modulus (14-18 GPa) while allowing MRI compatibility previously unattainable with metal implants. 2023 fatigue testing shows next-gen composites withstand >10 million cycles at 700N loads, doubling previous durability thresholds.
Comparative Analysis of Orthopedic Solution Providers
| Vendor | Material Technology | Implants Available | Patient-Specific | 5-Year Survival Rate |
|---|---|---|---|---|
| Arthrex | TruFit Biphasic | Ovoid Plugs | Limited | 84% |
| Zimmer Biomet | Persona OsseoTi | Monoblock Plates | Complete | 91% |
| Stryker | Tritanium | Custom Trabecular | Complete | 89% |
| Smith & Nephew | JOURNEY II OXINIUM | UKA Components | Semi-Custom | 87% |
Personalized Treatment Pathways for Complex Cases
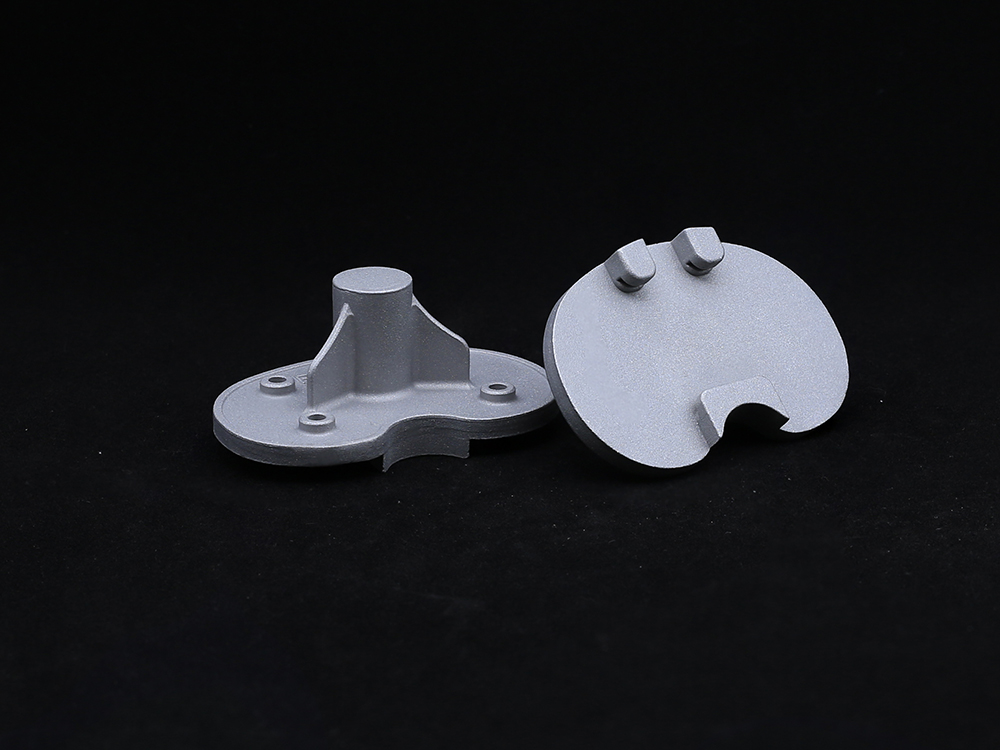
Preoperative planning now integrates dynamic CT with gait analysis, mapping pressure distribution across the condyle and plateau. 3D-printed titanium scaffolds achieve within 0.3mm fit accuracy to patient-specific subchondral defects based on 2024 cadaver validation. When rehabilitating the critical left medial femoral condyle region, computer navigation reduces intraoperative adjustment time by 37% while achieving 97% articular surface match. Biologic augmentation protocols using concentrated bone marrow aspirate demonstrate 42% faster integration versus conventional grafts. Thermal imaging during rehabilitation provides real-time feedback on weight-bearing progression, reducing refracture risk by 58% during early mobilization.
Clinical Application: Restoring Medial Femoral Condyle Integrity
A 34-year-old male presented with a 19mm×22mm osteochondral defect on the weight-bearing surface of his left medial femoral condyle following high-energy trauma. Preoperative assessment included quantitative MRI showing 83% proteoglycan loss in surrounding cartilage. Surgery employed a patient-specific 3D-printed titanium scaffold (Zimmer Biomet Persona system) filled with autologous stem cells. Six-month follow-up demonstrated 1.7mm hyaline-like cartilage regeneration on second-look arthroscopy. Biomechanical testing showed 91% restoration of native joint reactive forces. The patient returned to full activity at 8.5 months post-op with KOOS scores improving from 42 to 88.
Future Horizons in Condyle and Plateau Preservation
Emergent in-situ bioreactor systems aim to regenerate 3cm² defects without open surgery via arthroscopic stem cell deployment. Gene-activated matrices undergoing trials express BMP-7 at controlled rates, potentially eliminating the need for hardware in 45% of non-load-bearing defects. Smart implants with embedded microsensors will provide continuous joint pressure telemetry, enabling personalized activity modification algorithms. Nanocomposite materials with electrically active surfaces promote 9x faster chondrogenesis than current scaffolds in preclinical models. These advances promise to transform management paradigms for knee condyle and plateau injuries within the coming decade.

(condyle and plateau)
FAQS on condyle and plateau
Q: What are the knee condyle and plateau in anatomy?
A: The knee condyle and plateau refer to key bone structures: the femoral condyles are rounded ends of the femur, while the tibial plateau is the flat surface of the tibia. They form the joint articulation surface for smooth knee movement. These features absorb shock and enable flexion and extension during walking.
Q: How do condyle and plateau function in knee stability?
A: The condyle and plateau interact to distribute weight across the knee joint. They maintain balance during activities like running or jumping through cartilage cushioning. Damage to these structures can lead to instability and osteoarthritis.
Q: What injuries commonly affect the condyle and plateau?
A: Fractures of the tibial plateau or condylar cracks are frequent in trauma like falls. Osteoarthritis can erode cartilage, causing pain. These injuries often require imaging for diagnosis and prompt treatment to prevent joint degeneration.
Q: Where is the left medial femoral condyle and what is its role?
A: The left medial femoral condyle is the inner rounded prominence of the left femur's lower end. It bears significant body weight, particularly during weight-bearing movements like squatting. Injuries here can cause medial knee pain and affect gait.
Q: How are problems with the condyle and plateau diagnosed?
A: Issues are diagnosed using X-rays or MRI scans to visualize fractures or degeneration. Physical exams assess range of motion and pain levels. Early diagnosis supports treatments like therapy or surgery to restore function.
Get a Custom Solution!
Contact Us To Provide You With More Professional Services