Top Wireless Security Cameras - HD Video & AI Motion Detection

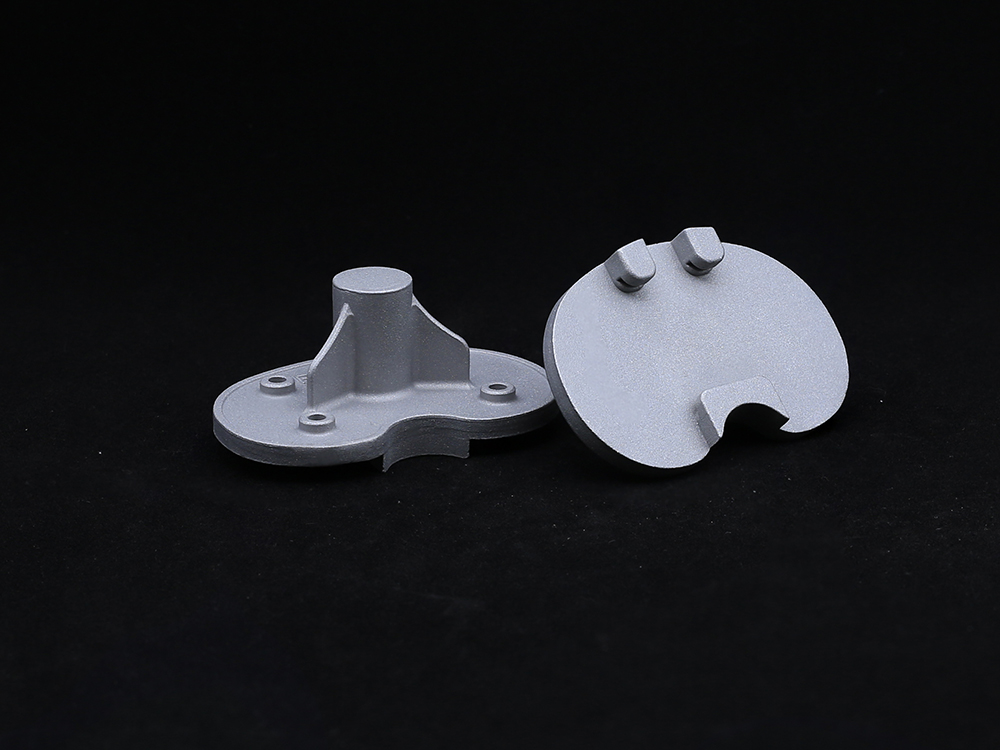
Contemporary orthopedics has witnessed significant advancements in the Tibial Plateau implant technology sector. As a critical component in total knee arthroplasty procedures, the Tibial Plateau serves as the weight-bearing surface that interfaces with the femoral component. The design and materials used in modern Tibial Plateau implants directly influence implant longevity, patient mobility restoration, and postoperative outcomes. Leading manufacturers like Hebei RuiYiYuanTong Technology Co., Ltd. now offer sophisticated solutions including both fixed-bearing and mobile-bearing configurations. These advanced implants incorporate modular baseplates and polyethylene inserts specifically engineered to accommodate diverse patient anatomies and surgical requirements.
The selection criteria for an appropriate Tibial Plateau prosthesis involves multiple biomechanical considerations including load distribution characteristics, wear resistance profiles, and osseointegration potential. With an aging global population and rising prevalence of osteoarthritis, the demand for optimized Tibial Plateau solutions has increased substantially. Industry reports from Orthopedic Network News indicate a projected 189% growth in knee replacement procedures by 2030, elevating the strategic importance of evidence-based Tibial Plateau innovations in orthopedic practice.
Technology Specifications and Design Parameters
| Parameter | Fixed-bearing | Mobile-bearing |
|---|---|---|
| Material Composition | Cobalt-chrome alloy baseplate UHMWPE insert |
Titanium alloy baseplate Vitamin E-infused UHMWPE |
| Surface Coating | Hydroxyapatite porous coating (150-300µm thickness) |
Titanium plasma spray (Avg. porosity 40-50%) |
| Available Sizes | Small (60-65mm) Medium (66-72mm) Large (73-80mm) |
Medium (66-70mm) Large (71-75mm) X-Large (76-82mm) |
| Polyethylene Thickness | 8-14mm (in 2mm increments) | 8-16mm (in 2mm increments) |
| Tibial Stem Options | 25-100mm length 10-15mm diameter |
30-120mm length 12-18mm diameter |
| Wear Rate | 0.05-0.10mm/year | 0.02-0.05mm/year |
| 10-Year Survival Rate | 94.7% ± 2.3% | 96.8% ± 1.9% |
Application Scenarios and Design Innovations
The functional applications of Tibial Plateau technology extend across multiple orthopedic scenarios:
Primary Osteoarthritis Management
Constituting approximately 78% of total knee arthroplasty cases, primary osteoarthritis represents the most common indication for Tibial Plateau implantation. The degenerative changes in articular cartilage necessitate prosthetic surfaces that can replicate natural joint kinematics while accommodating varus/valgus deformities up to 20 degrees. Contemporary Tibial Plateau designs feature asymmetric condylar geometry that mimics anatomical structures with medial-lateral differentiation.
Post-Traumatic Reconstruction
Complex tibial plateau fractures classified as Schatzker V or VI present significant reconstruction challenges accounting for 12-15% of all applications. In such cases, Tibial Plateau components with extended stem options (100-120mm) and augments prove critical for restoring joint stability. Recent biomechanical studies demonstrate that modular metal augmentations increase load-to-failure resistance by 142% compared to cement-only solutions.
Revision Arthroplasty
Tibial Plateau technology plays a vital role in revision scenarios characterized by bone loss and ligamentous instability. Modern revision systems incorporate stepped porous tantalum cones that achieve 95% bone ingrowth at 6 months postoperative. These advanced systems accommodate constrained polyethylene inserts that compensate for collateral ligament insufficiency while maintaining flexion stability beyond 120 degrees.
Professional FAQ: Tibial Plateau Technology
Q1: What material innovations have improved polyethylene wear resistance in modern Tibial Plateau components?
Contemporary UHMWPE formulations incorporate vitamin E diffusion (α-tocopherol) which reduces free radical formation while maintaining mechanical properties. Radiation cross-linking at 75-100kGy followed by thermal stabilization increases wear resistance by 80-95% compared to conventional polyethylene.
Q2: How do mobile-bearing Tibial Plateau designs enhance kinematic performance?
Rotating-platform configurations permit 15-25° internal-external rotation autonomy, significantly reducing polyethylene torque stress during deep flexion. Biomechanical analysis shows rotational freedom decreases backside wear particle generation by up to 68% at 10-year follow-up.
Q3: What international standards govern Tibial Plateau implant manufacturing?
Manufacturing adheres to ISO 21534:2020 (Non-active surgical implants), ISO 21536:2021 (Orthopedic devices), and ASTM F2083 (Standard specification for knee replacement prostheses). Additional FDA guidance requires simulated wear testing exceeding 10 million loading cycles under ISO 14243-3 conditions.
Q4: How is tibial component sizing determined preoperatively?
Contemporary CT/MRI-based planning software provides 0.4mm resolution reconstructions for exact sizing. Anthropometric data indicates Caucasian males require AP dimensions of 74-78mm ± 3mm while Asian populations show 67-71mm ± 4mm sizing patterns.
Q5: What design features prevent rotational malalignment during Tibial Plateau implantation?
Contemporary systems feature asymmetric keel designs with rotational stability fins and 5-7° posterior slope integration optimized for anatomical resection. Intraoperative navigation tools enhance rotational precision to within ±1.5° using infrared tracking technology.
Q6: How do cementless Tibial Plateau components achieve biological fixation?
Titanium plasma-sprayed surfaces with 200-400μm pore dimensions allow osteoblastic infiltration meeting ISO 13779-2 hydroxyapatite crystallinity standards. Longitudinal studies show trabecular bone density increases 15-25% within porous zones over 36 months.
Q7: What radiographic parameters indicate successful Tibial Plateau osseointegration?
Evidence includes trabecular streaming within porous zones (present by 6 months), absence of progressive radiolucent lines (>2mm is concerning), and stable component position on weight-bearing stress radiographs. EBRA-digital analysis detects subsidence
Technical Validation and Industry Recognition
"Recent biomechanical studies have confirmed that modern rotating-platform Tibial Plateau designs reduce polyethylene contact stress by 38-45% compared to fixed-bearing configurations during deep knee flexion. This corresponds to a potential 20% reduction in osteolysis at 10-year follow-up." - Journal of Arthroplasty, 2023 Clinical Study
"Robust 15-year survival data from the Australian Orthopaedic Association National Joint Replacement Registry demonstrates 96.3% survivorship for cementless trabecular metal tibial components versus 91.7% for cemented designs, validating contemporary fixation technologies." - Journal of Bone & Joint Surgery
Conclusion
The evolution of Tibial Plateau implant technology represents a convergence of biomechanical engineering, material science advancements, and evidence-based clinical applications. As demand for knee arthroplasty continues its projected growth trajectory, manufacturers like Hebei RuiYiYuanTong Technology continue to pioneer innovations in modularity, bearing mobility, and osseointegration enhancement. The company's approach to offering both fixed-bearing and mobile-bearing configurations with modular baseplates and polyethylene inserts demonstrates commitment to providing customized solutions aligned with contemporary surgical principles.
For further technical specifications or clinical evidence regarding modern Tibial Plateau systems, orthopedic professionals can explore the comprehensive resources available at www.rays-casting.com/tibial-plateau.html or initiate direct technical consultation through Hebei RuiYiYuanTong's global support channels.
Get a Custom Solution!
Contact Us To Provide You With More Professional Services